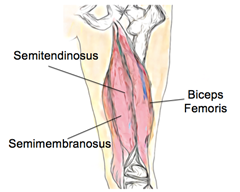
What are they?
The hamstrings are a large group of muscles, located at the back of the thigh. Their job is to bend the knee, move the hip backwards and stabilise the leg. The muscles can be injured at any point but are most vulnerable where the tendon and muscle fibres join together. This is a common injury for players of all sports that involve running, but particularly those that involve quick movements and kicking.
What are the causes?
As the hamstrings cross two large joints, they need to perform complicated movements, often activating suddenly and with great force. They are often stretched during a fall, large kick or sudden take-off. Factors that increase the chance of a tear, include poor flexibility and neural mobility. Other factors that contribute to hamstring injuries are muscle imbalances, abnormal lower limb biomechanics, fatigue, and inadequate warm-up. It seems, however, the biggest predictor of a future hamstring tear is a previous hamstring injury.
What are the symptoms?
The most common symptom of a torn hamstring is a sharp pain at the back of the thigh, often immediately after intense activity. There may also be swelling, bruising, difficulty walking and pain with knee movements. The symptoms of a hamstring tear are similar to many other conditions, as the lower back often refers pain to the back of the thigh, mimicking a hamstring tear.
Your physiotherapist can confirm that the pain is due to a torn hamstring and tell you how bad the tear is. Although not usually required, diagnosis can be confirmed by having an MRI or real-time ultrasound scan.
How can physiotherapy help?
Once a diagnosis has been made, the first step is to follow the R.I.C.E protocol (Rest, Ice, Compression, Elevation). During the first 48 hours, you should apply ice for 20 minutes every hour to reduce swelling and bruising. Consultation with your physio will include advice about your recovery, and when it is appropriate to return to sport. Your physiotherapist has many techniques that can promote healing and reduce scar tissue formation, which may include ultrasound, deep tissue therapy, laser, TENS and dry needling.
They will also prescribe an exercise program to return strength, flexibility and control to the muscle, getting you back to your sport quickly and safely. Due to the high chance of recurrence, rehabilitation is very important and usually takes 6-12 weeks. If the muscle is completely torn, surgery may be required before rehabilitation can start. Your physiotherapist will work with you to help you set goals to get you back to your favourite activities as soon as possible.
None of the information in this article is a replacement for proper medical advice. Always see a medical professional for advice on your individual injury.