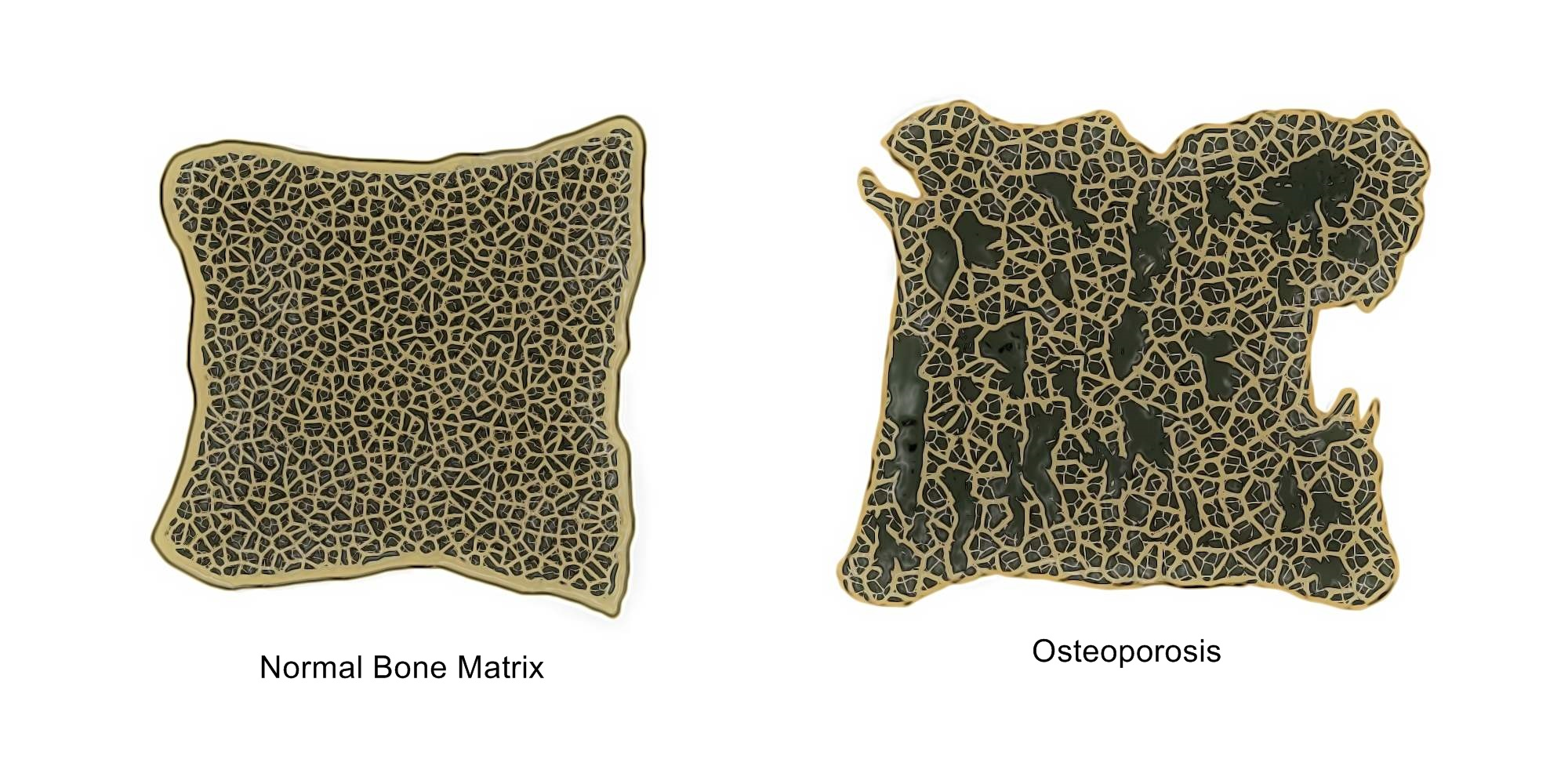
Osteoporosis is a condition characterized by very low bone mass or density. This is caused by the body either losing too much bone, not making enough or both. Osteoporotic bones become weak and fragile and can break from small forces that would normally be harmless.
In osteoporotic bones, as well as loss of bone density and mass, there may also be abnormal changes to the structure of the bone matrix, which further contributes to the bone weakness.
Osteoporosis is an extremely common bone disease and women are more affected than men. As it is a progressive disorder that worsens with age, while the disease process might begin earlier, the effects are usually only noticed and diagnosed in people who are 50 years and older.
What are the Signs and Symptoms?
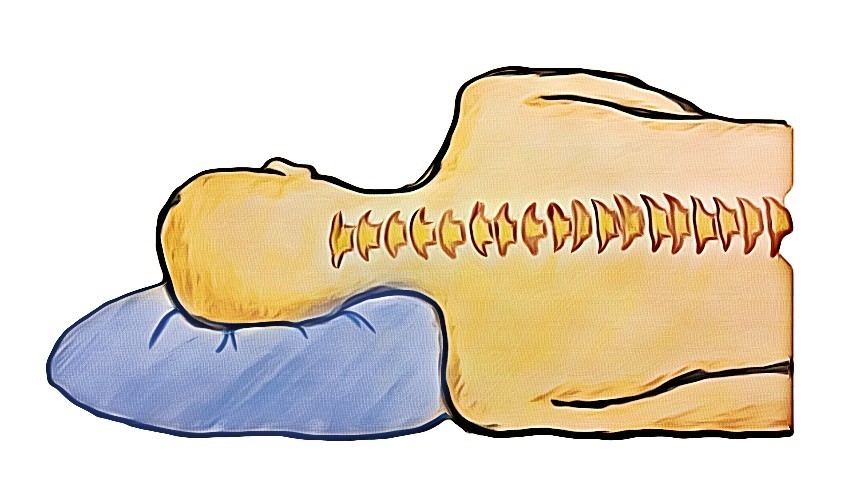
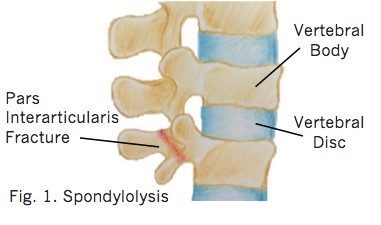
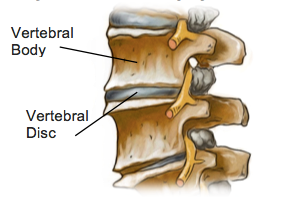
Often called a silent disease, many people with osteoporosis will have no idea that they have the disease, as there are no obvious symptoms. In fact, sometimes the first sign that an individual has osteoporosis is when the first bone is broken. Along with fractures, which are the most serious signs of this disease, osteoporosis can cause the upper back to become excessively hunched (itself often a result of spinal wedge fractures). There maybe widespread pain as bony tissue is increasingly unable to withstand normal forces.
Fractures are a serious problem, especially in the elderly population. Bone breaks due to osteoporosis occur most frequently in the wrist, spine or hip. When the spine is affected by osteoporosis, people may develop a hunched or stooped posture, which can itself lead to respiratory issues and places pressure on the internal organs. Osteoporosis can severely impact a person’s mobility and independence, which can have a huge impact on quality of life.
What Causes It?
As this is primarily a metabolic disorder, there are a variety of things that can cause osteoporosis. These factors either interfere with the body’s ability to either produce bone tissue, or encourage excessive breakdown. This can be anything from gastrointestinal conditions that prevent absorption of calcium, lack of dietary calcium or low levels vitamin D, which is essential for absorption of calcium.
Certain medications may also cause bone loss especially if they are taken for a long time or in high doses. A good example is the long-term use of steroids. Although steroids are used to treat various conditions, it has been proven that steroids can cause bone loss and eventually, osteoporosis.
As bones respond to force and weight bearing by building more bone, having a sedentary lifestyle or doing activities with low impact can also lead to osteoporosis. This has been shown to be an issue amongst professional swimmers and cyclists.
How Can Physiotherapy Help?
Physiotherapy can help you to improve your overall bone health, avoid or recover from fractures. Physiotherapy exercises can direct you to safely increase your weight bearing, which can help build bone mass. Balance training is also an important factor as this can reduce the risk of falls. Your physiotherapist can also educate you on how to adjust your lifestyle, at home or at work, to protect your bones and improve your posture.
None of the information in this newsletter is a replacement for proper medical advice. Always see a medical professional for advice on your individual condition.