Travel can be one of the most enjoyable aspects of life, however if a trip away comes with the risk of increased pain and soreness, the excitement can be thoroughly diminished. Many people will even avoid travel altogether if their symptoms are exacerbated too much by long seated periods. If you are unlucky enough to fall into this category, here are a few tips from your physiotherapist that might help make long trips a little more comfortable.
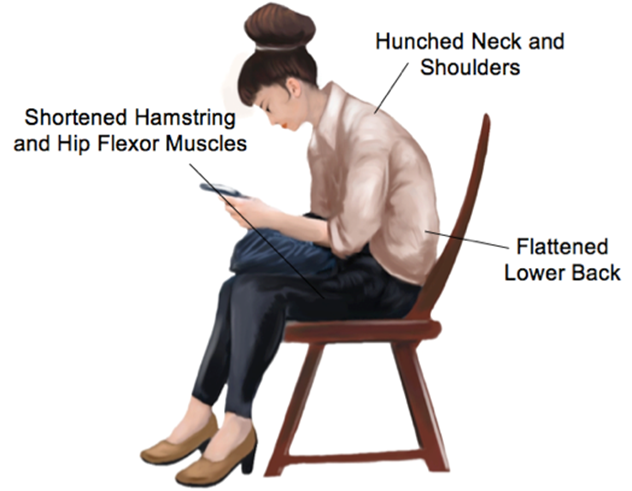
Lower back pain is the chief complaint of most travellers. To avoid low back pain, try the following tips:
1) Adjust the seat angle.
If you are able, tilt the seat slightly down towards your feet, not towards your hips. Ideally, your knees should be level with your hips, or even slightly lower. A footrest to lift your knees can also help.
2) Lift the height of the whole seat. This will assist with tip #1 by lifting the whole body away from the floor. When your hips are less bent, it is easier for your back to sit comfortably in an upright position.
3) Use a lower back support.
Many cars nowadays come equipped with in-built lumbar supports. Often this support is a generic design and not fitted for your specific shape or height. A proper lumbar pillow, or even a rolled towel in the small of the back, can be more effective in maintaining the natural arch of your spine. This relieves pressure through your intervertebral discs, spinal ligaments, and spinal muscles.
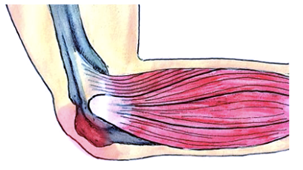
Neck discomfort is easier to improve when tips for lower back are implemented first. Some very easy tips to reduce neck pain are as follows:
1) Use a travel pillow.
If travelling on an airplane, try wearing the pillow backwards or sideways. This assists in supporting the head in a slightly better position when you rest or sleep, which helps to reduce the stress placed on the muscles, ligaments and joints within the neck.
2) Every hour, perform 10 chin tucks.
This is easiest to perform correctly if you sit tall and press your chin straight backwards, lengthening the back of your neck. Do not tuck the chin to the chest. This exercise stretches the small postural muscles at the base of the skull, relaxing them. The tips above are only suggestions. If you find they are helpful, continue performing them throughout your travels. However, if any of the above tips cause you pain or discomfort, it is advisable to seek your physiotherapist’s opinion.