Strengthen to Lengthen, Does It Work?
Improving flexibility by stretching is a core tenant of most exercise programs. We have all heard the adage to stretch and warm-up before exercise to help prevent injuries and there is no doubt that stretching can just feel amazing! It can be surprising to learn that sometimes, the answer to improving flexibility can actually come from strengthening muscles, not just stretching them.
Why is this?
The muscles of the body are primarily responsible for its movement. By contracting and shortening they move their attachments closer together or by relaxing they allow their attachment to move apart in a controlled manner. The stronger and more coordinated muscles are, the more efficiently muscles are able to move the body more precisely and against more resistance.
This likely comes as no surprise, however what you may not realise is that muscles also play a large role in providing stability to the body, particularly around the more flexible joints such as the hip and shoulder. If needed, they will often prioritise their role as stabilisers over that of movers.
What does that mean?
If muscles are too weak to allow safe and controlled movement when needed, they might ‘tighten up’ to provide the stability necessary to keep your body upright. The less movement through range, the less blood flow muscles will be receiving, which can also lead to reduced muscle health and greater risk of injury. Increasing the strength of muscles can allow them to relax and move more freely, improving flexibility.
One of the reasons why strengthening to improve flexibility may seem counter intuitive is because many of have experienced muscle pain and stiffness after a strength workout, which can add to the perception that strengthening muscles shortens them. This pain and stiffness is usually short lived, reducing over 48 hours as muscle tissues return back to normal.
Do any strengthening exercises work?
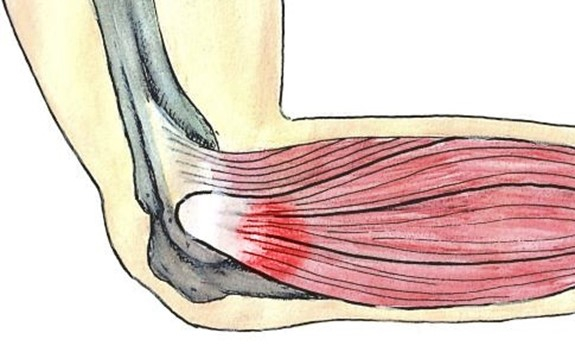
While improving strength and coordination may allow muscles to ‘relax’, there is one type of strengthening exercise that will actually physically lengthen muscles by creating new muscle cells. Eccentric exercises, or ‘controlled lengthening’ have been shown to have a very beneficial effects on muscle health, length and even improve tendon health. Having a targeted eccentric training program to strengthen muscles has been shown to improve flexibility and reduce injuries overall.
Ask your physiotherapist for tips on training muscles to their optimal health to promote flexibility. Your physiotherapist is able to assess any muscles for weakness and reduced length, giving you a targeted program to improve function and reduce injuries.