What is Ankylosing Spondylitis?
Ankylosing Spondylitis, a type of inflammatory arthritis, causes inflammation and pain in the spinal column as well as other joints in the body. The classic marker of Ankylosing Spondylitis is involvement of the sacroiliac joints, which are large joints connecting the pelvic bones to the sacrum in the lower back.
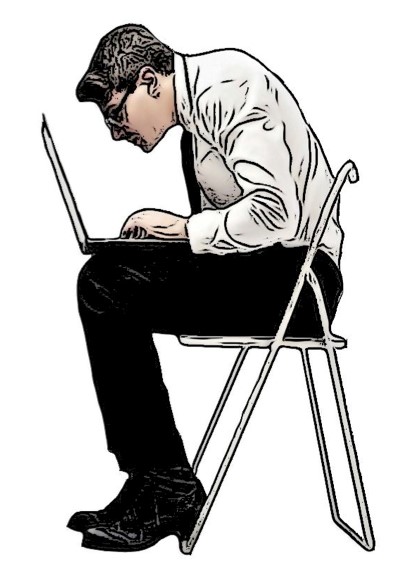
In many cases of Ankylosing Spondylitis, inflammation within the spinal column can cause new bone to begin forming between the vertebrae. Vertebrae are the individual bones that compose the spinal column. This leads the vertebrae to fuse in various areas, typically fusing the spine in flexed forward, immobile postures.
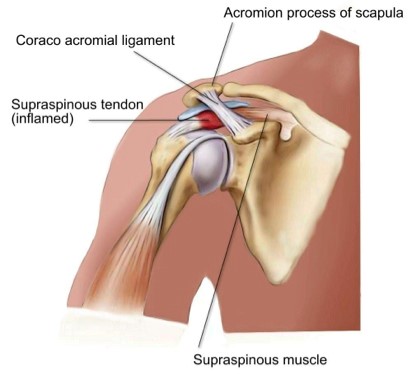
As Ankylosing Spondylitis progresses, other areas of the body may be affected. These areas include the smaller joints within the hands and feet, as well as the ribs and shoulders. In some instances, the disease can affect other systems of the body such as the skin, lungs and eyes.
The cause of Ankylosing Spondylitis is not clear, however there are markers and predisposing factors that may contribute to the development of the condition.
Genetics, environment and frequent gastrointestinal infections are among the pre-disposing factors. Men are more commonly affected than women and diagnosis tends to occur between the ages of 17 and 45 years.
What are the signs and symptoms?
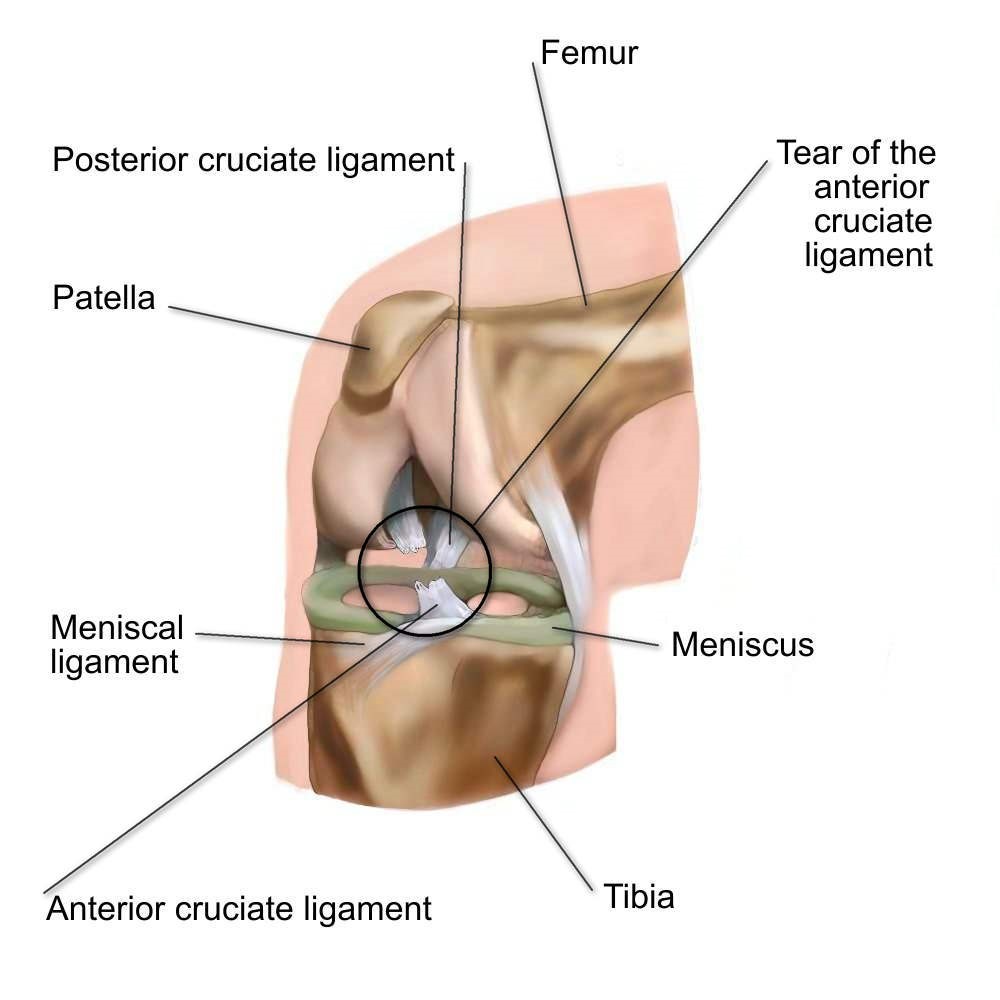
Back pain and stiffness are the two most common symptoms of Ankylosing Spondylitis. Other symptoms include neck and buttock pain, as well as pain in the smaller joints of the hands and feet. Tendons and ligaments may also be affected. Symptoms tend to be worse following periods of rest, and better following periods of activity. It is common for people to experience “flare-ups” and “remissions” of symptoms.
Severity of disease is patient-dependent. Some people with Ankylosing Spondylitis may experience discomfort in the spine from time to time, while others experience severe and debilitating symptoms at frequent intervals with minimal time in remission from symptoms.
Many people with ankylosing spondylitis do not seek medication attention, especially if the symptoms are mild. In these cases, the disease is not diagnosed until it has progressed, leading to increased pain and disability for the patient.
How can physio help?
Ankylosing Spondylitis responds well to physical activity. Your physiotherapist will assess your spinal movement and posture as well as strength and overall movement ability. They will assist you with performing appropriate stretches and strengthening exercises to maintain your posture, spinal strength and mobility. If your hands, feet, hips or shoulders are involved, they will also provide you with specific exercises to help maintain mobility and strength in those joints.
In many cases, people can participate in group exercise programs in a pool and on land. Exercising in a pool is beneficial due to the buoyancy factor; people do not have to weight bear on sore and inflamed joints, however are still able to stay physically active. Many studies have proven the positive benefits of exercise for those with Ankylosing Spondylitis, such as improved rib cage expansion when breathing, and improved posture of the upper back and neck. A physiotherapist is also able to implement other pain relieving treatments that can help to manage symptoms.
None of the information in this newsletter is a replacement for proper medical advice. It is important that you always see a medical professional for advice on your individual condition.
Please click the download button below to print out a free copy of our newsletter.


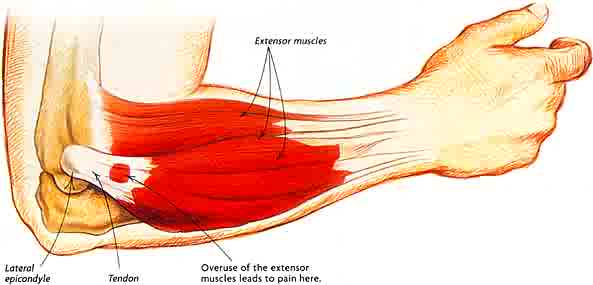
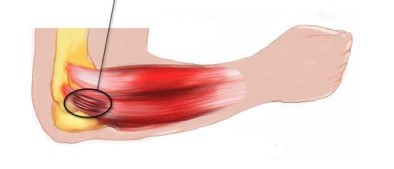 Tennis elbow can come on either suddenly, or develop gradually over time. The pain may begin with activity and quickly go away following activity in the early stages. As it progresses, it may be painful before and after activity, but ease while in use.
Tennis elbow can come on either suddenly, or develop gradually over time. The pain may begin with activity and quickly go away following activity in the early stages. As it progresses, it may be painful before and after activity, but ease while in use.

 Balance and stability are important skills that can help to prevent injury. Can you stand on one leg for 30 seconds without falling or wavering?
Balance and stability are important skills that can help to prevent injury. Can you stand on one leg for 30 seconds without falling or wavering?